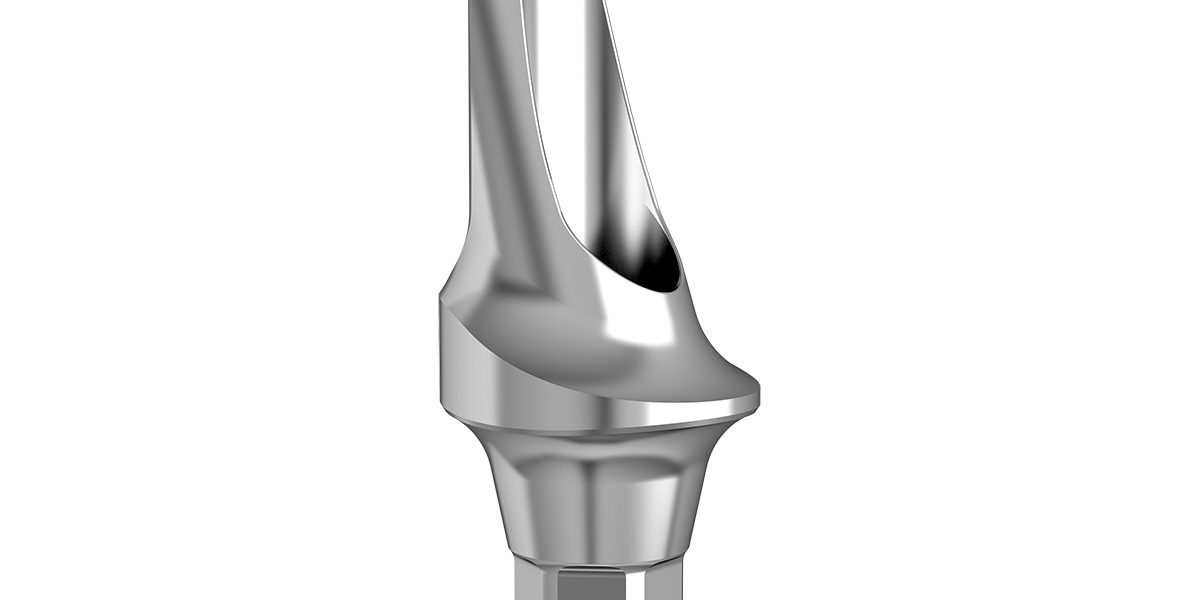
The abutment is an indispensable and critical component of the dental implant system, playing a vital role in the tooth restoration process. It precisely serves as a stable connecting bridge between the dental implant (a metal fixture surgically embedded into the jawbone) and the upper prosthesis or custom-made crown.
In terms of structure and function, the abutment acts like a carefully designed anchor. It is firmly attached to the implant and provides strong support and stability for the crown above. This ensures that the crown can be securely fixed in the oral cavity, allowing the patient to chew food naturally and speak clearly—just like using natural teeth—thus restoring both the normal function and aesthetics of the dentition.
Types of Dental Abutments
1. Conventional Prefabricated Abutment (Stock Abutment)
Standardized Design
Traditional abutments are industrially mass-produced and available in various fixed diameters (e.g., 3.5mm, 4.0mm, 5.0mm) and angulations (0°, 15°, 30°) to suit different implant systems. They are typically cylindrical or slightly tapered in shape, with surfaces processed via machining or anodizing.
Clinical Indications
- Simple anterior restorations: When alveolar bone conditions are favorable and adjacent teeth are in normal alignment, a stock abutment can be directly used for single-tooth restoration.
- Cost-effective solutions: Suitable for posterior restorations in patients with limited budgets or low esthetic demands, especially for short-term or transitional use.
- Emergency restorations: In immediate implant placement or provisional restoration cases, stock abutments allow for quick installation, shortening the treatment timeline.
Limitations
- Cannot fully match the patient’s individualized anatomy, which may result in unnatural gingival contours or food impaction.
- Limited angulation adjustment; poor adaptability for tilted implants (e.g., >15°).
2. Custom Abutment
Digitally Precise Manufacturing
Patient-specific oral data is acquired via intraoral scanning or stone models and used to design abutments through CAD/CAM technology. Materials are typically titanium alloy or zirconia, with zirconia being preferred in esthetic zones due to its high translucency.
Clinical Advantages
- Biomimetic design: Can replicate the natural emergence profile, cervical curvature, and occlusion of the original tooth, achieving a highly esthetic and natural-looking outcome.
- Micro-gap control: Provides a more precise implant-abutment connection, reducing bacterial colonization risk and lowering the incidence of peri-implantitis.
- Dynamic functional adaptation: Abutment height and angulation can be adjusted for patients with tight occlusion or bruxism, dispersing occlusal forces and enhancing long-term implant stability.
Typical Applications
- Immediate implant placement in the anterior region: Custom abutments can shape ideal interdental papillae, avoiding the “black triangle” issue.
- Full-arch edentulous restoration: In techniques like All-on-4, custom abutments optimize screw channel positions for easier long-term maintenance.
3. Special-Function Abutments
Angulated / Adjustable Abutments
- Design features: These abutments use ball joints or Morse taper connections at the implant interface, allowing directional adjustment within a certain range (typically ±15°–30°).
- Indications: Ideal for correcting tilted implants or avoiding critical anatomical structures (e.g., mandibular nerve canal).
Healing Abutments
- Temporary function: Used during the initial post-implant phase to guide gingival soft tissue healing and form an ideal emergence profile.
- Types: Available in various heights (e.g., 2mm, 4mm, 6mm) and shapes (flat or convex tops) depending on gingival thickness.
Emergence Profile Abutments
- Esthetic enhancement: For patients with thin gingival biotypes, preformed or custom convex-profile abutments can increase soft tissue volume and mask implant metal color.
4. Innovations in Materials and Connection Methods
One-Piece Abutment-Crown
- Integrated structure: The abutment and crown are fused into a single unit via laser welding or CAD/CAM milling, eliminating microleakage risks.
- Indications: Suitable for short-span fixed bridges in the posterior region or for patients with high hygiene demands.
Dynamic Abutment System
- Smart adaptation: Combined with digital impression technology, the abutment can be adjusted directly in the mouth for angle and height, eliminating the need for lab-side modifications and shortening treatment time.
5. Clinical Decision-Making Tree
- Esthetic demands: Zirconia custom abutments or emergence profile abutments are preferred in the anterior esthetic zone.
- Functional needs: Patients with tight occlusion or bruxism should be fitted with custom anti-rotation abutments.
- Cost considerations: Simple posterior restorations may use prefabricated abutments, but long-term maintenance costs should be evaluated.
- Anatomical limitations: For tilted implants or insufficient bone volume, angulated abutments and bone grafting techniques should be combined.
Through careful selection of the appropriate abutment type, clinicians can strike a balance between function, esthetics, and cost—ultimately achieving long-term success in implant restorations.
The Importance of Dental Abutments
Abutments are not only the physical link between implants and crowns but also a critical component in achieving function, esthetics, and long-term oral health. From the initial selection of biocompatible materials to final dynamic functional adaptation, every design detail directly impacts the success of implant restoration. With advancements in digital technology and material science, custom abutments are becoming the mainstream solution, offering patients more precise, reliable, and esthetic implant treatments.
1. Structural Support
Bridge Between Implant and Crown
The abutment connects the dental implant (an “artificial root” embedded in the jawbone) with the prosthetic crown via precise mechanical means—such as Morse taper, screw-retained, or cement-retained designs—forming a complete restoration unit. Its structural strength directly affects the fracture resistance of the implant, especially under occlusal forces. The abutment must effectively distribute stress to the surrounding bone to avoid localized overload, which could lead to bone resorption or implant loosening.
An “Adjuster” for Varying Anatomical Conditions
In cases of tilted implants, insufficient bone volume, or complex adjacent tooth relationships, abutments can be adjusted in angle (e.g., angulated abutments) or height (e.g., emergence profile abutments) to compensate for anatomical limitations. For example, in posterior tilted implant cases, a custom abutment can reposition the crown into proper vertical occlusion, avoiding occlusal interference.
2. Functional Realization
Transmission and Cushioning of Occlusal Force
A high-quality abutment should have a suitable elastic modulus to efficiently transfer masticatory force to the jawbone (promoting osseointegration), while absorbing part of the impact through material deformation to protect the implant–bone interface. For instance, titanium alloy abutments are the preferred choice for posterior functional restorations due to their excellent biocompatibility and mechanical properties, whereas zirconia abutments meet both esthetic and functional demands in the anterior region thanks to their high strength.
Dynamic Functional Adaptation
For patients with bruxism or tight occlusion, abutments can be reinforced for stability through microstructural designs (e.g., anti-rotation grooves) or by selecting stronger materials such as cobalt-chrome alloy. In addition, angulated abutments allow for post-restorative fine-tuning of crown position, optimizing occlusal contact and improving chewing efficiency.
3. Esthetic Outcome
Biomimetic Design of Gingival Contours
The emergence profile of the abutment must accurately replicate the cervical curve and soft tissue contours of natural teeth, guiding healthy papilla formation and preventing black triangles or gingival recession. For example, custom zirconia abutments, with their tooth-like color and translucency, can provide highly natural esthetic results through thin gingival biotypes—especially ideal for immediate implantation in the anterior zone.
Translucency and Color Matching of Materials
Zirconia abutments simulate the semi-translucent effect of enamel due to their high light transmission, while titanium abutments may require masking techniques such as opaquing or customized staining to avoid grayish gingival appearance. Moreover, the interface between abutment and crown must be seamless to avoid unnatural light reflection that gives an artificial look.
4. Long-Term Stability
Microgap Control and Bacterial Sealing
The microgap between the abutment and implant is a potential source of bacterial colonization and inflammatory reactions. Custom abutments, manufactured with digital precision, can reduce this gap to below 10μm, significantly lowering the risk of peri-implantitis. Studies show that implants restored with custom abutments have about 15% higher 5-year survival rates compared to conventional abutments.
Soft Tissue Attachment and Biological Seal
Surface treatments such as sandblasting, acid etching, or laser texturing on abutments promote gingival fibroblast attachment, forming a dense biological seal that blocks bacterial infiltration. Healing abutments, with preformed emergence profiles, guide the soft tissue to develop an ideal collar shape, laying the foundation for long-term oral health.
5. Complication Prevention
Avoiding Mechanical Complications
Stable abutment retention prevents loosening, detachment, or fracture of the crown, reducing the need for secondary repairs. For example, screw-retained abutments use controlled torque preload (typically 25–35 N·cm) to ensure long-term stability, while cement-retained abutments require strict isolation from saliva to prevent residual cement from causing inflammation.
Reducing Biological Complication Risks
Poorly designed abutments—such as those with excessive emergence profiles or incorrect angulation—can lead to food impaction, gingival inflammation, or occlusal trauma. By using digital surgical guides and dynamic navigation technology, clinicians can precisely plan abutment positions, ensuring alignment with adjacent and opposing teeth and promoting overall oral harmony.
How to Choose the Right Abutment
Compatibility with Implant Characteristics
- Angulation Adaptability: If the implant is angled more than 15°, use an angulated abutment or a customized abutment to correct axial deviation and prevent misalignment of the prosthesis.
- Interface Type: Choose an abutment connection compatible with the implant brand (e.g., Nobel Active, Nobel Parallel CC, Straumann, bion), such as internal hex, external octagon, or Morse taper.
- Diameter and Length: The abutment diameter should be slightly smaller than the implant platform diameter (typically 0.5–1mm smaller) to avoid stress concentration. The length must cover the gingival cuff and allow space for prosthetic restoration.
2. Aesthetic Requirements Grading
| Grade | Clinical Characteristics | Recommended Abutment |
|---|---|---|
| Level 1 | Posterior region, thick gingival biotype, low smile line | Traditional titanium abutment or prefabricated angulated abutment |
| Level 2 | Anterior region, medium smile line, normal gingival contour | Customized zirconia abutment or emergence profile abutment |
| Level 3 | Anterior region, thin gingival biotype, high smile line | Digitally customized abutment + soft tissue graft |
3. Functionality and Mechanical Performance
- Occlusal Force Distribution: In posterior regions, choose high-strength materials (such as cobalt-chromium alloy or zirconia). In anterior regions, both aesthetics and strength should be considered (e.g., titanium abutment + zirconia crown).
- Anti-Rotation Design: For patients with bruxism, the abutment should include anti-rotation features (e.g., grooves or reinforced screw-retained structure) to prevent prosthesis loosening.
- Microgap Control: Customized abutments can reduce the microgap at the implant-abutment interface to below 10μm, significantly lowering the risk of peri-implantitis.
Comparison of Abutment Types & Typical Clinical Applications
1. Stock Abutment (Traditional Prefabricated Abutment)
Advantages: Low cost, immediately available, suitable for standardized restorations.
Limitations: Limited angulation adjustment range (usually ±15°), cannot perfectly match personalized anatomical structures.
Typical Applications:
- Single-tooth posterior restorations with good bone conditions and low aesthetic demand.
- Temporary or transitional restorations (e.g., 3–6 months after immediate implantation).
2. Custom Abutment (Personalized Abutment)
Advantages: Fully adapts to patient-specific anatomy, excellent aesthetic outcomes, high long-term stability.
Limitations: Higher cost, 2–4 weeks processing time required.
Typical Applications:
- Immediate implantation and restoration in the anterior region (requires papilla guidance).
- Patients with thin gingival biotype (requires enhanced soft tissue thickness via abutment contour).
- Angulated implants or cases following bone augmentation (requires axis correction and stress distribution).
3. Angulated Abutment (Adjustable Abutment)
Advantages: Adjustable angle (±15°~30°), no additional fabrication needed, suitable for urgent restorations.
Limitations: Slightly lower long-term stability than custom abutments; may increase risk of microleakage.
Typical Applications:
- Implant angulation exceeds adjustment range of prefabricated abutments.
- Elderly patients or those with poor compliance needing fast restoration.
Future trends: Digital and intelligent selection tools
AI-assisted design: Analyze patient CBCT data through machine learning and automatically recommend the optimal abutment type and parameters.
Dynamic guide technology: Combined with 3D printing guides, an integrated process of abutment implantation and restoration production is achieved.
Biomaterial innovation: For example, nano-coated abutments can promote soft tissue attachment and reduce postoperative inflammatory reactions.
Conclusion
implant restorations. It requires a comprehensive evaluation of implant characteristics, aesthetic demands, functional requirements, and individual patient differences. With the widespread adoption of digital technologies, custom abutments are gradually becoming the mainstream choice. However, traditional abutments still hold irreplaceable value in certain clinical scenarios. Dentists should engage in continuous learning and clinical practice to fully understand the indications and limitations of each type of abutment, ultimately delivering implant solutions that provide functional, aesthetic, and biological benefits for their patients.